Leads on ECG: 12 Essential Facts You Must Know Now
Ever wondered how a simple ECG can reveal so much about your heart? It all comes down to the leads on ECG—each one capturing a unique electrical perspective of your heartbeat. Let’s dive into what makes them so powerful.
Understanding the Basics of Leads on ECG

Electrocardiography (ECG or EKG) is a cornerstone of cardiac diagnostics, offering a non-invasive window into the heart’s electrical activity. At the heart of this technology—literally—are the leads on ecg, which are not wires or physical connections, but rather specific views or angles of the heart’s electrical impulses. These leads allow clinicians to detect abnormalities in rhythm, conduction, and even structural issues like myocardial infarction.
The standard 12-lead ECG is the most widely used configuration in clinical settings. Despite its name, it doesn’t use 12 separate electrodes. Instead, it uses just 10 electrodes placed on the limbs and chest to generate 12 different electrical perspectives—or leads. Each lead measures the voltage difference between two points, providing a vector-based snapshot of the heart’s activity during each beat.
What Are Leads on ECG?
In ECG terminology, a “lead” refers to a specific recording channel that captures the electrical potential between two or more electrodes. These leads are mathematical derivations based on electrode placement and are designed to view the heart from different anatomical angles. For example, some leads focus on the inferior wall of the heart, while others look at the lateral or anterior surfaces.
It’s crucial to understand that leads are not the same as electrodes. Electrodes are the physical sensors placed on the skin, while leads are the calculated outputs derived from those electrodes. This distinction is fundamental when interpreting ECG tracings and diagnosing cardiac conditions.
Types of Leads: Limb vs. Precordial
The 12 leads are divided into two main categories: limb leads and precordial (chest) leads. The limb leads include six views—three standard (I, II, III) and three augmented (aVR, aVL, aVF)—which are derived from electrodes placed on the arms and left leg. These leads primarily assess the heart’s vertical and frontal plane activity.
leads on ecg – Leads on ecg menjadi aspek penting yang dibahas di sini.
On the other hand, the precordial leads (V1 to V6) are placed across the chest in specific intercostal spaces and provide horizontal plane views of the heart. They are especially useful in detecting anterior, septal, and lateral wall abnormalities. Together, these leads form a comprehensive 3D map of the heart’s electrical behavior.
Why Leads on ECG Matter in Diagnosis
The arrangement and interpretation of leads on ecg are critical for accurate diagnosis. For instance, ST-segment elevation in leads II, III, and aVF suggests an inferior myocardial infarction, while elevation in V1–V4 points to an anterior infarction. Misplacement of electrodes can lead to misinterpretation, emphasizing the importance of proper lead placement.
Moreover, certain leads are more sensitive to specific conditions. Lead II, for example, is often used for rhythm monitoring because it aligns well with the heart’s electrical axis. Similarly, lead V1 is invaluable for identifying right ventricular hypertrophy or bundle branch blocks.
“The 12-lead ECG is one of the most powerful diagnostic tools in cardiology—when interpreted correctly, it can save lives.” — Dr. Eric Topol, renowned cardiologist and digital medicine pioneer.
The Standard 12-Lead ECG Configuration
The standard 12-lead ECG is the gold standard for cardiac assessment in both emergency and outpatient settings. Its widespread use is due to its ability to provide a comprehensive view of the heart’s electrical activity from multiple angles. This configuration includes six limb leads and six precordial leads, each offering unique diagnostic insights.
Understanding how these leads are derived and what they represent is essential for healthcare professionals and students alike. The system was developed by Willem Einthoven in the early 20th century, earning him the Nobel Prize in Physiology or Medicine in 1924. His work laid the foundation for modern electrocardiography.
Limb Leads: I, II, III, aVR, aVL, aVF
The limb leads are recorded using electrodes placed on the right arm (RA), left arm (LA), right leg (RL), and left leg (LL). The right leg serves as an electrical ground and does not contribute to the lead recordings. Leads I, II, and III are known as the “Einthoven’s triangle” and are bipolar leads, meaning they measure the voltage difference between two limbs:
leads on ecg – Leads on ecg menjadi aspek penting yang dibahas di sini.
- Lead I: Measures voltage between LA and RA (LA – RA)
- Lead II: Measures voltage between LL and RA (LL – RA)
- Lead III: Measures voltage between LL and LA (LL – LA)
The augmented limb leads (aVR, aVL, aVF) are unipolar and use a single limb as the positive electrode while combining the other two as a reference. These leads enhance the signal and provide additional perspectives:
- aVR: Looks at the heart from the right shoulder
- aVL: From the left shoulder
- aVF: From the feet (inferior view)
These six limb leads collectively assess the heart’s activity in the frontal plane, helping identify axis deviations, inferior infarcts, and limb lead reversals.
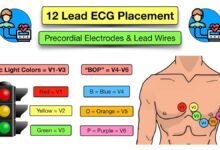
Precordial Leads: V1 to V6 Placement Guide
The precordial leads are placed directly on the chest and provide horizontal plane views of the heart. Their placement follows a standardized pattern:
- V1: 4th intercostal space, right sternal border
- V2: 4th intercostal space, left sternal border
- V3: Midway between V2 and V4
- V4: 5th intercostal space, midclavicular line
- V5: Anterior axillary line, same horizontal level as V4
- V6: Midaxillary line, same level as V4
These leads are crucial for detecting localized myocardial damage. For example, V1 and V2 are sensitive to septal infarcts, V3 and V4 to anterior wall issues, and V5 and V6 to lateral wall abnormalities. Accurate placement is vital—misplacement by even one intercostal space can alter the ECG interpretation significantly.
How Leads on ECG Create a 3D Electrical Map
By combining the frontal plane data from limb leads and the horizontal plane data from precordial leads, the 12-lead ECG constructs a three-dimensional representation of the heart’s electrical activity. This allows clinicians to localize the site of arrhythmias, conduction blocks, and ischemic changes with remarkable precision.
For example, during a myocardial infarction, the affected area of the heart becomes electrically silent or depolarized, creating a vector of injury current. This shows up as ST-segment elevation in the leads that “face” the damaged tissue. The pattern of involvement across multiple leads on ecg helps determine the infarct location and guides treatment decisions like thrombolysis or percutaneous coronary intervention (PCI).
leads on ecg – Leads on ecg menjadi aspek penting yang dibahas di sini.
Advanced algorithms and AI-powered ECG interpreters now use this 3D mapping to predict conditions like left ventricular dysfunction or even hyperkalemia with increasing accuracy. You can learn more about ECG interpretation at ECG Waves, a trusted educational resource.
Lead Placement Errors and Their Impact
Despite the standardized protocol, lead placement errors are surprisingly common in clinical practice. These mistakes can lead to misdiagnosis, unnecessary testing, or delayed treatment. Even experienced technicians can make errors, especially in emergency or high-stress environments.
Studies have shown that up to 40% of ECGs may have some degree of lead misplacement. The consequences range from subtle waveform changes to dramatic shifts that mimic life-threatening conditions like myocardial infarction or pulmonary embolism.
Common Mistakes in Limb Lead Placement
One of the most frequent errors is reversing the right and left arm electrodes. This can cause lead I to invert, making all other limb leads appear abnormal. For instance, P waves, QRS complexes, and T waves in lead I will be negative instead of positive, potentially leading to a false diagnosis of dextrocardia or limb lead reversal.
Another common issue is placing limb electrodes on the torso instead of the limbs, which alters the electrical reference and distorts the ECG. While sometimes done for patient comfort, this practice should be avoided unless using a modified protocol like the Mason-Likar system, which is designed for exercise stress testing.
Chest Lead Misplacement: Risks and Consequences
Precordial lead misplacement is equally problematic. Placing V1 and V2 too high or too low can mimic right ventricular hypertrophy or anterior infarction. Similarly, shifting V4–V6 laterally can create the appearance of lateral ischemia.
leads on ecg – Leads on ecg menjadi aspek penting yang dibahas di sini.
A particularly dangerous error is swapping V1 and V2 with V3 and V4, which can simulate a Brugada pattern—a condition associated with sudden cardiac death. Clinicians must always verify lead placement, especially when the ECG shows unexpected or life-threatening patterns.
How to Avoid Errors in Leads on ECG
To minimize errors, healthcare providers should follow strict protocols:
- Use anatomical landmarks (e.g., sternal angle, midclavicular line) to locate intercostal spaces
- Double-check electrode labels before recording
- Train staff regularly on proper ECG technique
- Use ECG machines with built-in lead reversal detection
Some modern ECG devices now include AI-assisted placement verification, alerting technicians to potential errors before the test is finalized. Resources like the American Heart Association offer detailed guidelines on proper lead placement.
Clinical Significance of Specific Leads on ECG
Each of the 12 leads on ecg has a unique clinical role. Understanding which leads correspond to which areas of the heart is essential for accurate diagnosis and treatment planning. This section explores the diagnostic power of key leads and how they guide clinical decisions.
Lead II and Rhythm Monitoring
Lead II is one of the most commonly used leads for monitoring cardiac rhythm. Its positive electrode is on the left leg and negative on the right arm, aligning closely with the heart’s natural electrical axis. This makes it ideal for visualizing P waves, which are crucial for determining the origin of a rhythm.
In atrial fibrillation, for example, lead II clearly shows the absence of P waves and an irregularly irregular rhythm. In heart block, the relationship between P waves and QRS complexes can be assessed with high clarity in lead II.
leads on ecg – Leads on ecg menjadi aspek penting yang dibahas di sini.
V1 and V2: Detecting Right-Sided and Septal Issues
Leads V1 and V2 are positioned over the right ventricle and interventricular septum. They are particularly useful in diagnosing right bundle branch block (RBBB), where a characteristic “rabbit ear” pattern (RSR’ complex) appears in V1.
These leads also help identify septal myocardial infarction, which shows as Q waves in V1–V2. Additionally, V1 is critical in diagnosing arrhythmias like atrial flutter, where “sawtooth” flutter waves are often most visible.
Leads V5, V6, and Lateral Wall Assessment
Leads V5 and V6, along with aVL and I, view the lateral wall of the left ventricle. ST-segment elevation or depression in these leads can indicate lateral ischemia or infarction. They are also important in assessing left ventricular hypertrophy (LVH), where tall R waves in V5–V6 combined with deep S waves in V1–V2 suggest increased left ventricular mass.
The Cornell voltage criterion for LVH uses the sum of the R wave in aVL and the S wave in V3. This demonstrates how specific leads on ecg are used in diagnostic formulas.
Special ECG Lead Configurations
While the standard 12-lead ECG is the most common, there are specialized lead systems used in specific clinical scenarios. These configurations provide additional diagnostic information when the standard leads are insufficient.
Right-Sided ECG Leads (V3R to V6R)
In suspected right ventricular infarction—often associated with inferior MI—right-sided leads (V3R to V6R) are placed on the right chest. ST elevation in V4R is a key indicator of right ventricular involvement and may guide fluid management and reperfusion therapy.
leads on ecg – Leads on ecg menjadi aspek penting yang dibahas di sini.
These leads are temporary and not part of the standard 12-lead set, but their use can be life-saving in acute coronary syndromes.
Posterior Leads (V7 to V9)
Posterior myocardial infarction is often missed on standard ECGs because the posterior wall isn’t directly viewed. Leads V7, V8, and V9 are placed on the back (V7 at left posterior axillary line, V8 at left scapular line, V9 at left paraspinal line) to detect ST elevation in posterior MI.
Alternatively, tall R waves and ST depression in V1–V3 can be indirect signs of posterior infarction, prompting the use of posterior leads for confirmation.
Esophageal and Intracardiac Leads
In electrophysiology studies, specialized leads are used to record electrical activity from within the heart. Esophageal leads, for example, are inserted into the esophagus (which lies close to the atria) to better visualize atrial activity in cases of suspected atrial tachycardia or flutter.
Intracardiac leads, used during ablation procedures, provide millimeter-precise recordings from within the atria and ventricles, guiding the treatment of complex arrhythmias.
Interpreting ECG Patterns Across Leads
ECG interpretation is not about analyzing one lead in isolation but understanding how patterns evolve across multiple leads on ecg. This holistic approach allows for accurate localization of pathology and differentiation between similar-looking conditions.
leads on ecg – Leads on ecg menjadi aspek penting yang dibahas di sini.
ST-Segment Changes and Myocardial Infarction
ST-segment elevation is a hallmark of acute myocardial infarction. The leads showing elevation indicate the infarct location:
- Inferior MI: II, III, aVF
- Anterior MI: V1–V4
- Lateral MI: I, aVL, V5–V6
- Septal MI: V1–V2
Reciprocal ST depression in opposite leads (e.g., ST depression in aVL during inferior MI) further supports the diagnosis. The pattern across leads helps rule out mimics like pericarditis, which typically shows diffuse ST elevation.
Q Waves and Infarct Localization
Pathological Q waves—deep and wide—indicate prior myocardial infarction. Their presence in specific leads helps determine the infarct site:
- II, III, aVF: Inferior wall
- V1–V2: Septal
- V3–V4: Anterior
- I, aVL, V5–V6: Lateral
However, Q waves can also be normal in certain leads (e.g., aVR, III), so context is key.
Axis Determination Using Limb Leads
The electrical axis of the heart is determined by analyzing the QRS complex in the limb leads. A normal axis ranges from -30° to +90°. Deviations can indicate conditions like left axis deviation (common in left anterior fascicular block) or right axis deviation (seen in right ventricular hypertrophy).
Using the quadrant method—assessing positivity in leads I and aVF—clinicians can quickly estimate the axis. For example, positive in I and aVF = normal axis; negative in I, positive in aVF = right axis deviation.
leads on ecg – Leads on ecg menjadi aspek penting yang dibahas di sini.
Advancements in ECG Lead Technology
Modern technology is transforming how leads on ecg are used. From wearable devices to AI-driven analysis, the future of ECG is becoming more accessible, accurate, and predictive.
Wearable ECG Monitors and Lead Simplicity
Devices like the Apple Watch and AliveCor KardiaMobile use fewer electrodes to simulate standard leads. The KardiaMobile, for example, generates a single-lead ECG comparable to lead I, allowing users to detect atrial fibrillation at home.
While not a replacement for 12-lead ECGs, these tools increase early detection of arrhythmias and improve patient engagement. They demonstrate how simplified lead systems can still provide valuable clinical data.
AI and Machine Learning in Lead Analysis
Artificial intelligence is being integrated into ECG interpretation software to detect subtle patterns invisible to the human eye. Algorithms can now predict conditions like asymptomatic left ventricular dysfunction, pulmonary hypertension, and even sleep apnea from standard leads on ecg.
A landmark study published in Nature Medicine showed that an AI model could predict mortality from ECG data alone, outperforming traditional risk scores. Learn more about AI in cardiology at Nature Medicine.
Future Trends: Vector ECG and 3D Mapping
Emerging technologies like vectorcardiography (VCG) and high-resolution 3D ECG mapping are pushing the boundaries of cardiac diagnostics. VCG plots the magnitude and direction of electrical vectors in three dimensions, offering superior spatial resolution compared to standard ECG.
leads on ecg – Leads on ecg menjadi aspek penting yang dibahas di sini.
These systems may soon be integrated into routine care, allowing for earlier detection of ischemia and more precise localization of arrhythmogenic substrates.
What are leads on ECG?
Leads on ECG are the electrical viewpoints of the heart generated by placing electrodes on the body. The standard 12-lead ECG uses 10 electrodes to create 12 different views (6 limb leads and 6 precordial leads) that help diagnose heart conditions by analyzing the heart’s electrical activity from multiple angles.
How many leads are there in a standard ECG?
A standard ECG has 12 leads: 6 limb leads (I, II, III, aVR, aVL, aVF) and 6 precordial leads (V1 to V6). These are derived from 10 electrodes placed on the limbs and chest.
What does ST elevation in leads II, III, and aVF indicate?
leads on ecg – Leads on ecg menjadi aspek penting yang dibahas di sini.
ST elevation in leads II, III, and aVF typically indicates an acute inferior myocardial infarction. These leads view the inferior wall of the heart, and ST changes suggest ischemia or infarction in that region.
Can lead placement affect ECG results?
Yes, incorrect lead placement can significantly alter ECG results, leading to misdiagnosis. For example, reversing arm electrodes can mimic dextrocardia, and misplaced chest leads can simulate anterior infarction. Proper training and verification are essential.
What are posterior ECG leads used for?
Posterior ECG leads (V7, V8, V9) are placed on the back to detect posterior myocardial infarction, which may not be visible on standard 12-lead ECGs. They help identify ST elevation in the posterior wall of the left ventricle.
Understanding leads on ecg is fundamental to mastering ECG interpretation. From the basic limb and precordial configurations to advanced applications in AI and wearable tech, these electrical viewpoints provide invaluable insights into cardiac health. Proper placement, accurate interpretation, and awareness of limitations ensure that ECG remains a powerful tool in modern medicine. As technology evolves, the diagnostic potential of ECG leads will only continue to grow, offering earlier detection and better outcomes for patients worldwide.
leads on ecg – Leads on ecg menjadi aspek penting yang dibahas di sini.
Further Reading: