Leads ECG Placement: 10 Critical Steps for Accurate Diagnosis
Understanding leads ecg placement is essential for healthcare professionals aiming to deliver precise cardiac assessments. Proper positioning ensures reliable data, aiding in early detection of heart conditions and improving patient outcomes.
Leads ECG Placement: The Foundation of Cardiac Monitoring

Electrocardiography (ECG or EKG) is one of the most widely used diagnostic tools in cardiology. It records the electrical activity of the heart over time, allowing clinicians to detect arrhythmias, ischemia, infarctions, and other cardiac abnormalities. At the core of an accurate ECG reading lies correct leads ecg placement. Misplaced electrodes can lead to misdiagnosis, delayed treatment, or unnecessary interventions.
What Are ECG Leads?
ECG leads are not individual wires but rather combinations of electrodes that measure voltage differences between specific points on the body. A standard 12-lead ECG uses ten electrodes placed strategically to generate twelve different views (leads) of the heart’s electrical activity. These include six limb leads and six precordial (chest) leads.
- Each lead provides a unique angle of the heart’s electrical vector.
- The system is based on Einthoven’s triangle and the hexaxial reference system.
- Understanding the spatial orientation of each lead helps interpret waveforms accurately.
Why Leads ECG Placement Matters
Inaccurate electrode positioning—even by a few centimeters—can distort the morphology of the P wave, QRS complex, and ST segment. For example, misplaced V1 and V2 electrodes can mimic right bundle branch block patterns or mask signs of anterior myocardial infarction.
“A misinterpreted ECG due to poor lead placement can be as dangerous as no ECG at all.” – Dr. William A. Zoghbi, Past President of the American Society of Echocardiography
Studies have shown that up to 40% of routine ECGs contain some degree of lead misplacement, particularly in the precordial leads. This highlights the need for standardized training and continuous quality control in clinical settings.
Understanding the 12-Lead ECG System
The 12-lead ECG system is designed to provide a comprehensive view of the heart from multiple angles. Despite its name, it uses only 10 physical electrodes: four on the limbs and six on the chest. The “12 leads” are derived mathematically from these electrode inputs.
Limb Leads: I, II, III, aVR, aVL, aVF
The limb leads monitor the heart’s electrical activity in the frontal plane. They are divided into two groups: the standard bipolar limb leads (I, II, III) and the augmented unipolar limb leads (aVR, aVL, aVF).
- Lead I measures voltage between the right and left arms.
- Lead II (commonly used in monitoring) goes from right arm to left leg.
- Lead III completes the triangle from left arm to left leg.
- aVR, aVL, and aVF are unipolar leads that use a central terminal as reference.
Proper leads ecg placement on limbs ensures that these vectors are recorded accurately. Electrodes should be placed on the fleshy parts of the limbs, avoiding bony prominences or areas with muscle movement.
Precordial (Chest) Leads: V1–V6
The chest leads provide horizontal plane views of the heart and are crucial for detecting regional abnormalities such as anterior, lateral, or septal infarcts.
- V1 is placed in the fourth intercostal space at the right sternal border.
- V2 is at the fourth intercostal space at the left sternal border.
- V3 is midway between V2 and V4.
- V4 is in the fifth intercostal space at the midclavicular line.
- V5 is at the anterior axillary line, same horizontal level as V4.
- V6 is at the midaxillary line, level with V4 and V5.
Errors in precordial lead placement are among the most common mistakes in ECG performance. For instance, placing V4 too high or too lateral can alter the R-wave progression and mimic pathology.
Step-by-Step Guide to Correct Leads ECG Placement
Accurate leads ecg placement requires attention to anatomical landmarks, patient positioning, and electrode adherence. Below is a detailed step-by-step guide to ensure precision.
Preparation: Patient and Equipment Setup
Before applying electrodes, prepare both the patient and equipment. Explain the procedure to reduce anxiety, which can cause muscle tremors and interfere with the tracing.
- Ask the patient to lie flat in a supine position, arms relaxed at the sides.
- Ensure the room is warm to prevent shivering.
- Clean the skin with alcohol wipes to remove oils and dead skin cells.
- Shave excessive chest hair if necessary to improve electrode contact.
Use high-quality, conductive electrodes designed for single-use to minimize impedance and motion artifact.
Locating Anatomical Landmarks
Correct identification of anatomical landmarks is critical for consistent leads ecg placement.
- The angle of Louis (sternal angle) is key for locating the second rib, which helps identify the fourth intercostal space.
- Palpate down from the sternal angle to find the second intercostal space, then count down to the fourth.
- The midclavicular line runs vertically from the midpoint of the clavicle.
- The anterior and midaxillary lines are identified by asking the patient to raise their arms slightly.
Using anatomical landmarks rather than arbitrary measurements ensures reproducibility across different body types and repeated tests.
Electrode Application Sequence
Follow a systematic sequence to avoid confusion:
Place RA (right arm) electrode on the right forearm, distal to the shoulder.Place LA (left arm) on the left forearm.RL (right leg) and LL (left leg) go on the lower limbs, typically near the ankles.Position V1 and V2 first, using the fourth intercostal space at the sternal borders.Locate V4 before V3 and V5–V6, as it serves as the anchor point.Place V4 in the fifth intercostal space at the midclavicular line.
.Place V3 midway between V2 and V4.Align V5 with V4 at the anterior axillary line.Place V6 at the midaxillary line, horizontal with V4 and V5.Double-check each position before initiating the recording.Misplacement of V4 is particularly common and can significantly affect interpretation..
Common Errors in Leads ECG Placement and How to Avoid Them
Despite its routine use, leads ecg placement is often performed incorrectly. Recognizing and correcting common errors is vital for diagnostic accuracy.
Misplaced Precordial Leads
One of the most frequent errors is incorrect placement of chest leads, especially V1 and V2. Placing them in the third or fifth intercostal space can mimic arrhythmias or obscure true pathology.
- V1 and V2 too high: May simulate atrial abnormalities or Brugada pattern.
- V1 and V2 too low: Can mask right ventricular hypertrophy or posterior MI.
- V4 placed laterally: Alters R-wave progression, mimicking anterior infarct.
To avoid this, always locate the angle of Louis and count ribs downward. Use a marking pen if needed to confirm positions before attaching electrodes.
Reversed Limb Electrodes
Arm-lead reversal (swapping RA and LA) is surprisingly common and produces characteristic changes:
- Inversion of P waves, QRS complexes, and T waves in leads I and aVL.
- Lead II and III appear swapped.
- aVR and aVL may show abnormal positivity.
Right and left leg reversal usually has minimal effect on the tracing since the legs are electrically similar. However, right arm and left leg reversal can simulate dextrocardia.
“Limb lead reversals are often unrecognized but can lead to incorrect axis determination and misdiagnosis of myocardial infarction.” – Source: National Center for Biotechnology Information (NCBI)
Incorrect Patient Positioning
The patient should be lying flat, not sitting up or reclining. Changes in body position alter the heart’s orientation, affecting lead vectors.
- Upright positioning can shift the heart downward, altering QRS axis.
- Arm tension or crossed limbs increase baseline noise.
- Respiratory motion can cause wandering baseline, especially in emphysematous patients.
Ensure the patient breathes normally and remains still during the recording.
Special Considerations in Leads ECG Placement
Certain patient populations and clinical scenarios require modifications to standard leads ecg placement protocols.
Obese Patients and Large Breasts
In patients with large breasts, precordial leads must be placed on the chest wall, not on breast tissue, to avoid signal attenuation.
- Lift the breast gently to locate the costal margins and intercostal spaces.
- Use extra-long lead wires or extensions if needed.
- Mark positions with a pen before electrode application.
For obese patients, consider using adhesive gel pads or suction electrodes to maintain contact.
Patients with Amputations or Limb Injuries
When limbs are missing or injured, alternative sites must be used while minimizing distortion.
- For missing arms, place electrodes on the upper abdomen or shoulders, keeping symmetry.
- Document the modified placement clearly on the ECG tracing.
- Use vector correction formulas if available, or interpret with caution.
In such cases, a 15-lead ECG or posterior leads may be more informative.
Pregnant Women and Pediatric Patients
Pregnancy elevates the diaphragm, shifting the heart upward and to the left. This affects R-wave progression and axis, but standard leads ecg placement remains unchanged.
- No modification in electrode placement is required.
- Be aware of normal physiological changes like sinus tachycardia and ST-T changes.
- In pediatrics, use smaller electrodes and adjust spacing proportionally.
For neonates and infants, limb electrodes can be placed on the torso to avoid limb movement.
Advanced Techniques: Posterior and Right-Sided ECGs
Standard 12-lead ECGs may miss posterior or right ventricular infarctions. Additional leads can enhance diagnostic yield.
Posterior Leads (V7–V9)
Used to detect posterior myocardial infarction, which may not show ST elevation in standard leads.
- V7: Fifth intercostal space at the left posterior axillary line.
- V8: Same level at the tip of the scapula.
- V9: Paravertebral area, left of the spine.
ST elevation in V7–V9 with reciprocal changes in V1–V3 suggests posterior MI. These leads are recorded using the same chest electrode after repositioning.
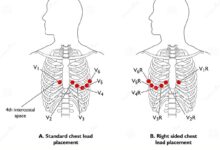
Right-Sided Leads (V3R–V6R)
Essential in suspected right ventricular infarction, often associated with inferior MI.
- V3R: Mirror image of V3 on the right side.
- V4R: Fifth intercostal space at the right midclavicular line (most sensitive).
- V5R and V6R: Right anterior and midaxillary lines.
ST elevation in V4R is a strong predictor of right ventricular involvement and guides fluid management in acute MI.
“Adding right-sided leads in inferior STEMI increases diagnostic sensitivity for right ventricular infarction by over 50%.” – American Heart Association Guidelines
Training and Quality Assurance in Leads ECG Placement
Despite its simplicity, leads ecg placement is a skill that requires ongoing education and supervision.
Standardized Training Programs
Hospitals and clinics should implement structured training for all staff involved in ECG acquisition.
- Include hands-on practice with anatomical models and live patients.
- Teach landmark identification and common pitfalls.
- Use competency checklists and periodic re-evaluation.
Simulation-based training has been shown to improve accuracy and retention.
ECG Quality Audits
Regular audits of ECG tracings can identify systemic issues in leads ecg placement.
- Review tracings for signs of lead reversal or misplacement.
- Provide feedback to technicians and nurses.
- Implement corrective actions when error rates exceed 5%.
Some institutions use automated software to flag potential placement errors based on waveform morphology.
Role of Technology in Improving Accuracy
Advancements in ECG technology are helping reduce human error.
- Smart electrodes with placement sensors are under development.
- Digital ECG machines now include lead integrity checks.
- AI-powered systems can detect lead reversals and suggest corrections.
While technology aids accuracy, it cannot replace foundational knowledge of proper leads ecg placement.
Interpreting ECGs with Suspected Lead Misplacement
When reviewing an ECG, clinicians must be able to recognize signs of incorrect leads ecg placement to avoid diagnostic errors.
Clues to Limb Lead Reversal
Several patterns suggest limb electrode swaps:
- Lead I with inverted P waves and QRS complexes: Suggests LA-RA reversal.
- aVR upright instead of inverted: May indicate limb reversal.
- Lead II and III switched: Compare PR intervals and QRS morphology.
If reversal is suspected, repeat the ECG with correct placement rather than attempting to “transpose” the leads mentally.
Identifying Precordial Misplacement
Abnormal R-wave progression or unexpected Q waves may indicate misplaced chest leads.
- Loss of R-wave progression in V1–V3: Could be due to V4 placed too laterally.
- Deep S waves in V1–V2: May result from low placement of V1/V2.
- Exaggerated R waves in V1: Suggests posterior MI or dextrocardia, but consider lead misplacement first.
Always correlate ECG findings with clinical presentation and consider repeating the test if placement is questionable.
When to Repeat the ECG
Indications for repeating an ECG due to suspected leads ecg placement errors include:
- Inconsistent findings with patient symptoms.
- Sudden, unexplained changes from prior ECGs.
- Presence of classic misplacement patterns (e.g., reversed P axis in lead I).
- Poor signal quality or excessive artifact.
Repeating the ECG with careful attention to technique often resolves diagnostic uncertainty.
What is the correct placement for V1 in leads ecg placement?
V1 is placed in the fourth intercostal space at the right sternal border. This position is critical for assessing right-sided heart activity and R-wave progression.
What happens if ECG leads are placed incorrectly?
Incorrect leads ecg placement can lead to misdiagnosis, such as mimicking myocardial infarction, arrhythmias, or chamber enlargement. It may also mask real pathology, delaying treatment.
How can I verify correct leads ecg placement?
Verify placement by locating anatomical landmarks (e.g., angle of Louis), using consistent measurement techniques, and checking for expected waveform patterns. Training and peer review also improve accuracy.
Are there alternatives to standard 12-lead ECG placement?
Yes, in special cases like dextrocardia or limb amputations, modified placements are used. Posterior (V7–V9) and right-sided leads (V3R–V6R) are also employed for specific diagnoses.
Can technology help prevent leads ecg placement errors?
Yes, modern ECG machines include lead integrity monitoring, and AI tools can detect reversals. However, human expertise in proper placement remains essential.
Accurate leads ecg placement is a cornerstone of reliable cardiac diagnosis. From proper electrode positioning to recognizing common errors, every step impacts the quality of the ECG. By following standardized protocols, investing in training, and leveraging technology, healthcare providers can ensure that ECGs deliver the insights needed for optimal patient care. Mastery of leads ecg placement isn’t just a technical skill—it’s a critical component of clinical excellence in cardiology.
Further Reading: